Piles
Piles, also known as hemorrhoids, are swollen blood vessels in the rectum or anus caused by excessive pressure. They can result in discomfort, itching, pain, and bleeding during bowel movements. Piles are categorized as internal or external, depending on their location. Common causes include constipation, prolonged sitting, or straining. Effective treatment options range from lifestyle changes to medical interventions.

Types of piles:
- Internal Piles: Located inside the rectum. Usually painless due to a lack of pain-sensitive nerves in the rectum. May cause bleeding during bowel movements or protrusion outside the anus during straining (prolapsed piles).
- External Piles : Form under the skin around the anus. Can cause significant pain and discomfort due to the presence of pain-sensitive nerves. May lead to swelling, itching, or a lump near the anus. Can form a blood clot (thrombosed piles), causing severe pain and a hard, swollen lump.
- Prolapsed Piles : Occurs when internal piles extend outside the anus. May cause discomfort, irritation, or soiling due to mucus discharge. Requires manual adjustment in moderate cases or surgical intervention in severe cases.
- Thrombosed Piles : A subtype of external piles where blood pools and clots inside the hemorrhoid. Symptoms include intense pain, swelling, and bluish discoloration. Requires immediate medical attention for pain relief and clot removal.
Symptoms of piles:
- Rectal Bleeding: Bright red blood during or after bowel movements, often noticed on toilet paper or in the toilet bowl.
- Pain or Discomfort : Pain during defecation or sitting for long periods, especially with external piles.
- Itching or Irritation: Persistent itching around the anus due to swelling or mucus discharge.
- Swelling Around the Anus: Presence of lumps or swelling near the anal area, which may be tender or painful.
- Mucus Discharge: A slimy discharge from the anus, leading to discomfort or soiling of undergarments.
- Prolapse: Internal piles may protrude from the anus during bowel movements and retract afterward or require manual repositioning.
- Incomplete Bowel Movements: A feeling that the bowel hasn’t emptied completely after defecation.
- Thrombosed Piles: External hemorrhoids can form clots, causing severe pain and hard lumps near the anus.
Causes of piles:
- Chronic Constipation: Straining during bowel movements increases pressure on rectal veins, causing swelling and the formation of piles.
- Chronic Diarrhea: Frequent bowel movements irritate the rectum and anus, potentially leading to hemorrhoids.
- Prolonged Sitting: Sitting for extended periods, especially on the toilet, puts extra pressure on rectal veins.
- Low-Fiber Diet: A diet lacking in fiber leads to harder stools, making bowel movements more difficult and contributing to straining
- Obesity: Excess body weight, especially around the abdomen, increases rectal pressure, elevating the risk of piles.
- Pregnancy: Hormonal changes and the weight of the uterus during pregnancy can exert pressure on the rectal veins.
- Heavy Lifting: Regularly lifting heavy objects can strain the rectal and anal area, leading to hemorrhoids.
- Aging: As tissues weaken with age, the risk of developing piles increases, particularly after the age of 50.
- Genetic Factors: A family history of piles may increase the likelihood of developing them due to inherited vein weaknesses.
- Poor Bathroom Habits: Spending excessive time on the toilet, such as while reading or using a phone, can stress rectal veins.
- Sedentary Lifestyle: Lack of physical activity contributes to poor digestion and increased pressure in the rectal area.
- Liver Diseases: Conditions affecting the liver, like cirrhosis, can increase venous pressure, contributing to hemorrhoid development.
- Anal Intercourse: This activity can cause trauma to the rectal area, potentially leading to piles.
- Dehydration: Insufficient water intake can harden stools, making bowel movements more difficult and painful.
- Excessive Coughing or Sneezing: Persistent coughing or sneezing exerts pressure on abdominal and rectal veins, increasing the risk.
- Alcohol and Spicy Food: Excessive consumption irritates the digestive tract, worsening symptoms.
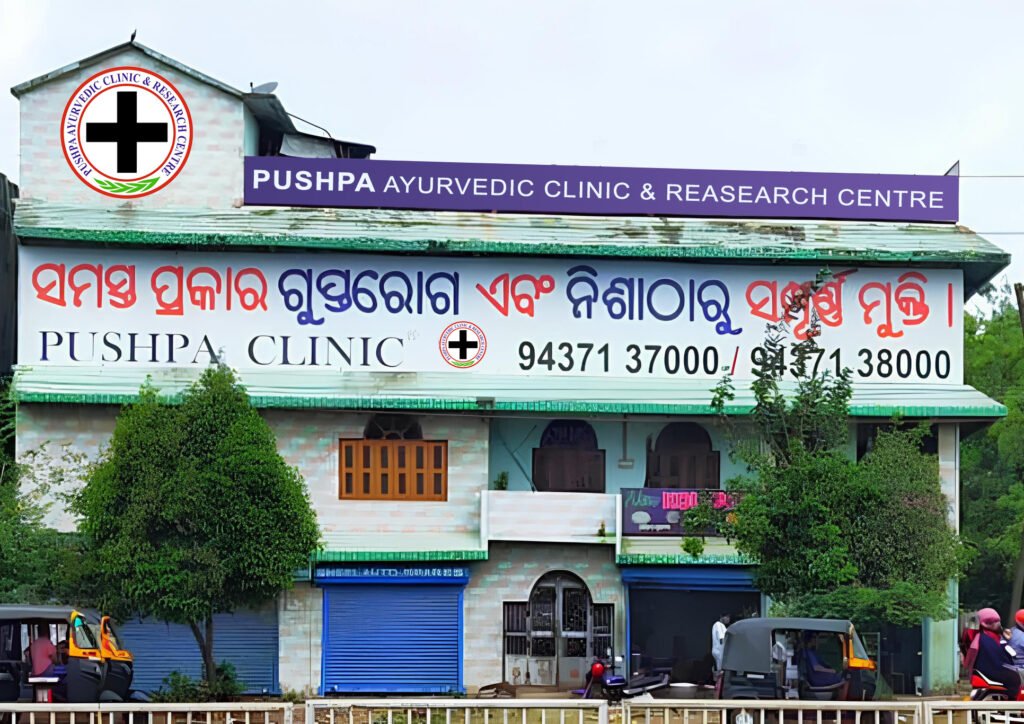
Treatment at Pushpa Ayurvedic Clinic & Research Centre :
- Detailed Diagnosis: Comprehensive consultation to identify the root cause of piles. Use of ancient Ayurvedic methods for accurate assessment.
- Customized Medicine Course: A three-month Ayurvedic treatment plan tailored to the patient's condition. Medicines made from natural herbs with no side effects.
- Dietary Guidelines: Personalized diet chart to promote healing and prevent recurrence. Recommendations to improve digestion and reduce strain during bowel movements.
- Lifestyle Modifications: Suggestions for yoga and exercises to enhance blood circulation. Guidance on avoiding triggers like prolonged sitting or heavy lifting.
- Non-Surgical Treatment Options: Use of Ayurvedic therapies effective treatment. Application of herbal ointments and oils for pain relief.
- Continuous Monitoring: Regular follow-ups to track progress and ensure effective treatment. Timely reminders for subsequent medicine purchases to complete the treatment.
- Focus on Complete Cure: Holistic approach to address the root cause and ensure long-term relief. Emphasis on natural healing to restore overall health.
- Patient Education: Awareness sessions on maintaining gut health. Tips to prevent recurrence of piles through healthy habits.